Breast cancer is the most dangerous and prevalently most common cancer incidence across the globe. Recent statistics unveil the brutal facts of breast cancer with the spectre of this disease and it may affect every treatment phase of life.
But amidst this higher prevalence and hurtful incidence of breast cancer—one in seven women in the UK is affected by Breast Cancer—is likely to develop this disease.
An Outlook of Breast Cancer Incidence
The phenomenal progression of breast cancer in the UK, USA, Europe, Africa, and Asia, has firmly set itself as a global health concern.
An estimated 56,500 new cases of female breast ductal carcinoma in situ (DCIS) and 310,720 cases of invasive disease in 2024 paint a depressing yet real picture. Alarmingly, statistics suggest that about 42,250 women diagnosed with breast cancer will die from the disease – so this figure demands more attention and denumerable preventive actions. Globally, 2.3 million women developed breast cancer in 2022, resulting in 670,000 were died from this.
According to the WHO, global breast cancer burden inequities are striking, based on the Human Development Index (HDI). For example, in mostly very high HDI countries, approximately 1 in 12 diagnosed women will be at a lifetime risk of developing invasive breast cancer. Additionally, 1 in 71 women from high HDI countries will die from breast cancer incidence and 1 in 48 could die in low HDI countries from it.
✌️ Future Predictions
This estimate has shown a 13% projected drop-in breast cancer mortality rates in the UK between 2023-2025 and 2038-2040. So, NHS initiatives have drawn a patient-centric cancer screening approach that might yield excellent results.
However, there could be around 11,400 breast cancer deaths annually in 2038-2040, which highlights the significance of continued achievements in fighting against the disease. Particularly, higher mortality rates among females in deprived areas in England are more common, and there is an urgent need for focused interventions and equitable breast cancer screening machine access, mostly in rural England.
What is Breast Cancer?
Breast cancer (BC) occurs when abnormal breast cells mutate into cancerous cells, multiply, and form tumours.
If one can’t notice or remains unchecked, the tumours have become malignant and cancerous lesions spread to other organs of the body and become deadly.
Breast cancer cells uncontrollably grow in milk ducts (or glandular tissue) and turn malignant (cancerous). This is most earliest form (in situ) of breast cancer and can easily be detected in the early stages. If cancer cells have grown into the surrounding breast tissue (invasion), these tumours are more likely to develop lumps or bumps.
Furthermore, when invasive cancers can spread to nearby organs like the brain, bones, lungs, liver, lymph nodes, or other organs, it’s referred to as metastasis BC or stage four breast cancer. Metastasis can be life-threatening and fatal.
This clinical expression of metastasis in a major organ is generally the final stage of cancer growth and can be life-threatening or a major culprit in cancer-related mortality. Treatment depends on the individual cancer type and its spread. Surgery, radiation therapy, and medications are the combined versions of the treatment.
Breast Cancer Check Machine

Most epidemiological studies hint at a complex interaction of factors in breast cancer – including genetics, lifestyle changes, socioeconomic status, hormonal, genetic (family history of breast cancer), and unequal access to healthcare infrastructure.
So, it’s very clear among many underdeveloped countries that breast cancer incidence has been growing in numbers. However, the easy accessibility and application of the most effective breast cancer check 3D breast imaging technology, regular screening, and knowledge of self-breast examinations could have potentially improved survival rates.
Yet, challenges still go on, especially in rural areas where accessibility to regular breast cancer screening services remains a big concern.
The Promise to Inclusive Approaches and Research Methodology

Several inclusive NHS Breast Screening Programmes have been initiated to help identify breast cancer early stage across the UK and invited women aged between 50 to 70 registered under their local GPs for weekly breast mammogram screening every 3 years taken of each breast. But, access to remote areas of the UK, but still lacks easy accessibility to breast cancer screening.
However, the incidence of early-onset (younger women) breast cancer is rising, so doctors have suggested the screening age should be lowered among BRCA1 or BRCA2 genes with a higher risk of BC are more commonly seen among younger women regardless of tumour molecular subtype.
Who is at a Higher risk of Breast Cancer?
Mostly females are commonly affected by breast cancer. Around, 99% of breast cancers may be seen among women and merely 0.5–1% among men.
Certain combinations of factors raise the chance of developing breast cancer risk, including associated factors, such as getting older, higher obesity, excessive consumption of alcohol & tobacco, hereditary breast cancer (BRCA1 or BRCA2 gene) around 5–10% cases of BC are hereditary, excessive radiation exposure, and HRT (Hormone replacement therapy) or postmenopausal hormone therapy.
In roughly 50% of breast cancer cases, the only risk factors are being female and older than 40. Certain inherited mutations among BRCA1, BRCA2 genes, and PALB2 Mutation are likely develop breast cancer.
Signs & Symptoms of Developing Breast Cancer
The absence of symptoms in early-stage cancer has mostly gone unnoticed, hence weekly breast screening plays a key role in early detection.
The common signs and symptoms of breast cancer can be included:
- Mastitis or breast swelling, painless
- Saggy breasts, change in breast anatomy
- Inflammatory breasts or dimpling
- A sudden change to darker-coloured nipples or areola
- Bloody Nipple discharge.
Anyone, if experiences a breast lump that is not normal, should get it checked by a doctor, regardless of the pain.
The Application of Koning vera Breast Cancer Screening UK

Koning Vera Breast cancer screening is a revolutionary 3D imaging device for the early detection of malignant breast tumours or any non-ass-like abnormal breast tissue, less than 4mm in size microcalcifications or masses.
This breast cancer checks machine offers less mammogram-like discomfort due to zero compression of breasts, therefore, no painful breast screening experience, producing real 3D images of the breasts in less the 7 seconds, and significantly low-dose radiation levels.
USA-based Koning Corporation has made this revolutionary device, now it has an FDA-approved breast cancer check machine. Its exceptional spatial resolution and real isotopic 3D images will not let any tiny-sized cancer lesions be hidden in dense breast tissues.
So, 3D images of the breasts could improve clinicians’ visualisation of the entire breasts. These real-time highly accurate images of the breasts correctly characterise breast lesions and offer primary treatment procedures once any abnormal clinical findings or tissue growth are noticed.
The Limitation of Mammogram Breast Cancer Screening
Traditionally, mammograms have been used in breast cancer screening, despite it has many limitations. These limitations include the chances of false-positive mammograms, showing abnormalities without the presence of breast cancer.
Consequently, additional testing such as rapid breast CT, MRI, ultrasound tests, or biopsies are often required to confirm the presence of breast lesions. These processes could cause lots of patient discomfort and hazards. Repeated breast CT due to false cancer recall require additional imaging, and excessive radiation exposure may cause radiation-induced breast cancer, which is very common.
The advent of the Koning Vera machine marks a significant change from these conventional practices, offering a more accurate and comfortable alternative. So, patient comfort is a higher priority.
Expert Testimony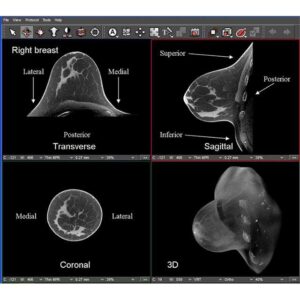
Medical experts have praised the state-of-the-art Koning Vera 3D breast imaging as breast cancer screening machine is seemingly correct and exceptionally accurate in early-stage breast cancer lesion detection and diagnostics. This superior digital breast tomosynthesis captures a 360-degree overview of the breasts.
This endorsement of the applications and non-invasive breast imaging technology shall improve radiologists’ ability to see and classify breast abnormalities in breast cancer screening and detection methods.
Conclusion
Koning Vera Breast Cancer Screening UK is currently available to give a patient-centric breast screening approach to UK citizens. So, it’s best time to recall the advantages of an advanced breast cancer check machine and NHS, private healthcare institutions, local GPs, patient advocates and NHS-affiliated trusts, should consider adopting this state-of-the-art technology, so patients get the benefit of a more comfortable and reliable breast screening experience.